Many hidden dangers of sleep apnea are mostly unknown. Sure, it’s easy to find the symptoms of sleep apnea, but what about the long-term side effects?
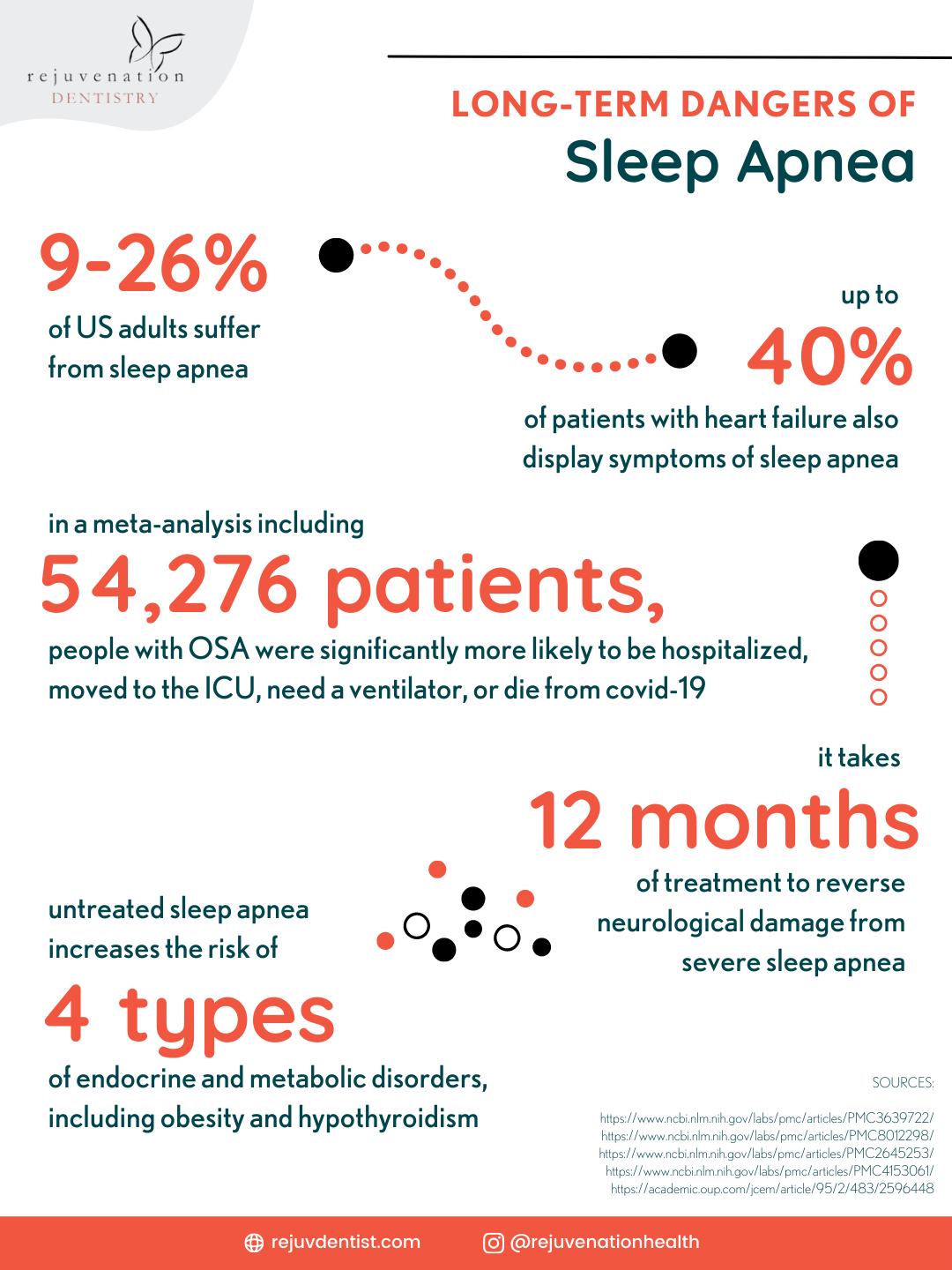
An estimated 9% to 26% of adults in America suffer from sleep apnea, and many cases go undiagnosed. Since untreated sleep apnea can lead to major long-term side effects, getting a healthcare professional to diagnose sleep apnea is vital.
Symptoms of Sleep Apnea
The common symptoms of sleep apnea are:
- Disrupted breathing during sleep
- Labored breathing while asleep
- Loud snoring, gasping, choking, and/or snorting
- Lower sleep quality for a bed partner
- Nighttime teeth grinding (AKA sleep bruxism)
- Morning headaches
- Irritability
- Difficulty concentrating
- Sore throat (usually caused by your snore)
- Dry mouth (which leads to poor oral health)
- Frequent urination at night
- Higher risk of automobile accidents
- Decreased job/school performance
- Excessive daytime sleepiness (primarily in adults)
- Attention-deficit hyperactivity disorder symptoms (primarily in children)
If you or a loved one is exhibiting warning signs of sleep apnea, seek medical advice right away. Diagnosing sleep apnea should be done sooner rather than later, so you and your bed partner can get a good night’s sleep and invest in a healthy future.
The main method of diagnosing sleep apnea is a sleep study that measures breathing, brain activity, oxygen levels, and other factors that may indicate you suffer from sleep apnea.
Causes of Sleep Apnea
To understand the causes of sleep apnea, you first must know that there are 3 types of sleep apnea, each with their own causes.
3 types of sleep apnea:
- Obstructive sleep apnea (OSA) — This is caused by a blockage in your upper airway, usually by your tongue or relaxed soft tissues, leading to temporary lapses in breathing. OSA is the most common form of sleep apnea. When people say “sleep apnea”, they usually mean OSA.
- Central sleep apnea (CSA) — This is caused when your brain fails to properly control respiration muscles, resulting in slower, shallower breathing. This may be brought on by certain medications or a stroke.
- Mixed sleep apnea — This is when you suffer from both OSA and CSA at the same time. It’s also known as “complex sleep apnea”.
What is the primary cause of sleep apnea? The primary cause of obstructive sleep apnea is that your tongue is too big for your mouth. You are at a higher risk for this sleep disorder if you deal with obesity, alcohol abuse, tobacco use, or if sleep apnea runs in your family.
In order to treat this root cause, I recommend the DNA appliance, which gradually, painlessly, naturally stretches the arches of your teeth. Not only can this allow enough room for your tongue in order to cure OSA, but patients also report the DNA appliance improves the look of their smile.
The main causes of central sleep apnea are stroke, high altitude-associated low oxygen levels, and taking certain drugs like oxycodone.
Common risk factors for sleep apnea include:
- Obesity
- Male gender
- Older age
- Black, Hispanic, and Native American race/ethnicity
- Tobacco use
- Excessive alcohol consumption
- Nasal congestion
- Large neck circumference
- Anatomical abnormalities
- Hormone abnormalities
- Chronic stress
- Genetics, family history
- Enlarged tonsils and adenoids (primarily in children)
Side Effects of Sleep Apnea
What are the long term effects of sleep apnea? Untreated sleep apnea and the resulting sleep deprivation are associated with surprising and devastating health risks.
The following medical conditions and other issues are just some of the side effects linked to untreated sleep apnea:
- Heart disease
- Respiratory dysfunction
- Brain abnormalities
- Infertility
- Oral health problems (bruxism/teeth grinding, cavities, periodontal disease, etc.)
- Obesity, weight gain
- Type 2 diabetes
- Liver problems
- Behavioral changes
- Depression
- ADHD symptoms (primarily in children)
- Lower IQ (primarily in children)
Effects on the Cardiovascular System
Even the most skeptical healthcare professionals know that sleep apnea is linked with a higher risk of cardiovascular dysfunction.
Sleep apnea may affect both your heart (“cardio”) and your circulatory system (“vascular”).
What does sleep apnea do to your heart? Long-term cardiovascular effects of untreated sleep apnea include:
- High blood pressure (hypertension)
- Irregular heartbeat (arrhythmia)
- Atrial fibrillation
- Heart attack
- Heart failure
Elevated muscle sympathetic nerve activity (MSNA) leads to hypertension and the risk of cardiovascular mortality. Since MNSA is typically elevated during sleep apnea, this is a prevailing theory as to why sleep apnea is so often linked to heart disease.
Up to 40% of people with diagnosed heart failure are referred for a sleep study because they show signs of sleep apnea.
One study revealed that diagnosing and treating sleep apnea before surgery significantly reduced postoperative cardiovascular complications.
Effects on the Respiratory System
Sleep apnea can have negative effects on your respiratory system.
Since sleep apnea deprives your body of much-needed oxygen while asleep, symptoms of asthma and chronic obstructive pulmonary disease (COPD) may worsen for apnea sufferers.
Sleep apnea might “increase the risk of respiratory complications and acute respiratory distress syndrome” in surgical candidates.
Although research is just emerging, it also seems possible that people with obstructive sleep apnea are at a greater risk of complications from covid. A review of studies including 54,276 patients found that patients with OSA were more likely to be hospitalized, moved to the ICU, put on a ventilator, and die from covid-19.
Specifically, OSA may contribute to hypoxemia (low blood oxygen levels), the cytokine storm, pneumonia, and even kidney injury.
Effects on the Nervous System
Your nervous system includes the brain and spinal cord. Untreated sleep apnea has been shown to impair cognitive function because it interferes with the nervous system.
Individuals with sleep apnea have been shown to have demonstrable functional and anatomical changes in various brainstem regions. One study shows that 6 months on a CPAP machine led to the complete reversal of those brain changes.
A 2014 study published in the journal Sleep shows that severe, untreated sleep apnea is linked to impairments in:
- Cognition
- Mood
- Daytime alertness
In that 2014 study, 12 months of CPAP treatment were needed to reverse the physiological damage to the brain caused by sleep apnea.
Several studies reveal that sleep apnea leads to reductions in cognitive function, attention, and even memory.
Effects on the Endocrine System
Patients with sleep apnea often experience altered hormone levels. Hormones are regulated by the endocrine system. Treating sleep apnea may reverse neuroendocrine dysfunction.
Individuals with sleep apnea have low growth hormone levels, without any other specific reason for the deficiency.
Hypothyroidism, an endocrine disorder, may lead to sleep apnea. However, sleep apnea can, in turn, cause other endocrine disorders.
Sleep apnea is associated with higher risk of endocrine disorders like polycystic ovary syndrome (PCOS) and hypogonadism.
Effects on the Reproductive System
Sleep apnea can negatively affect your reproductive system and reduce your sexual desire.
In men, this may contribute to erectile dysfunction. Animal studies indicate that sleep apnea may impair male fertility.
A 2019 retrospective study on over 4,000 Taiwanese women reveals that having sleep apnea puts females at higher risk for infertility. This may be due, in part, to the fact that endocrine disorders that cause infertility are more common in sleep apnea.
Other studies show that treating sleep apnea leads to improvements in testosterone levels, independent of weight loss.
Effects on Oral Health
Sleep apnea can have some nasty effects on your oral health, like:
- Dry mouth
- Tooth decay, cavities
- Gingivitis, periodontitis
- Teeth grinding (AKA bruxism)
- Increased risk of TMJ
For obvious reasons, sleep apnea often results in dry mouth. And dry mouth is the breeding ground for harmful bacteria that cause tooth decay and gum disease.
Less obviously, sleep apnea can lead to teeth grinding. When you stop breathing while asleep, your brain needs to wake you up for a moment, so you can start breathing again. The way your brain does this is by grinding your teeth together.
This works to wake you up so you’re breathing again, but it wreaks havoc on your dental health.
Not only can teeth grinding lead to jaw soreness, it can cause damage to your teeth and/or dental restorations.
Also, if your dentist identifies signs of teeth grinding, this may be an early indication of sleep apnea that prompts you to schedule a sleep study with a qualified sleep specialist.
Treatment of Sleep Apnea
Most common sleep apnea treatment options:
- Daytime-nighttime appliance (DNA)
- CPAP therapy (continuous positive airway pressure)
- APAP or BiPAP therapy
- Oral appliances (such as MAD or TRD)
- Adenotonsillectomy (mainly for children)
- Mouth taping (mainly for adults)
- Certain medications
- Quitting smoking
- Avoiding alcohol
- Weight loss through regular exercise and healthy diet
- Surgery
Some of these treatment options address the underlying cause (such as the DNA appliance), but others may simply address symptoms to improve quality of life just as long as you’re taking that treatment.
If you are living with sleep apnea, you should seek a diagnosis then a treatment plan as soon as possible.
Click here now to set up your appointment right away! Rejuvenation Dentistry’s offices are located in beautiful East Hampton and Manhattan. We empower our patients to take control of their whole-person health, including sleep problems like obstructive sleep apnea.