Jaw Cavitations
Treating Jaw Cavitations for Whole-Body Health
Jaw cavitations are lesions within the jawbone that harbor toxins and bacteria. The causes are not always known but may include blood flow blockage, certain medicines, medical procedures, long-term alcohol use, injury, or increased bone pressure. These cavitations are more severe than cavities but can be challenging to detect, even with X-rays, as they may not cause noticeable symptoms. However, it is crucial to treat them as they can lead to infection and immune dysfunction, impacting your overall well-being and health.
Understanding The Problem
Cavitations of the jaw may or may not cause pain. This raises the risk of a patient suffering from this condition for years without even knowing it. The problem is not just dead bone; it is what forms around it. The absence of healthy tissue facilitates the accumulation of bacteria, fungi, and parasites.
There are links between dental cavitations and other serious forms of disease such as heart disease, autoimmune diseases, HIV infection, sickle cell, pancreatitis, Gaucher’s disease, and others. Treating cavitations are therefore key for whole body health.

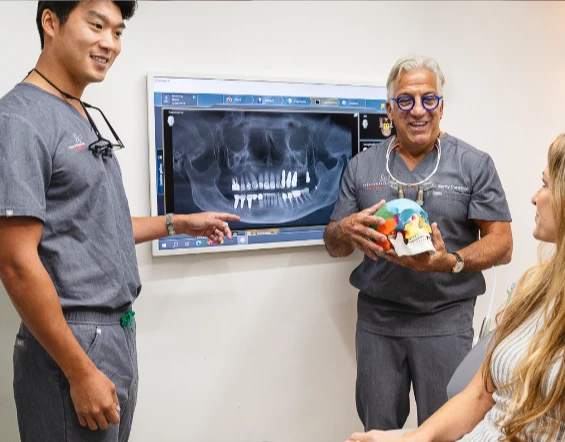
The 4-Step Curatola Jaw Cavitation Protocol
“Jaw cavitations have been poorly understood and widely untreated, yet may be one of the greatest threats to systemic health. Critical advances in diagnosis and treatment of these stealth infections have proven highly effective in supporting the resolution of chronic inflammation and the improvement of the innate immune system”
Dr. Curatola’s 4-step protocol includes assessment, pathology sampling, disinfection and debridement of necrotic bone and finally bone regeneration.The pathology results specifically is an invaluable tool to understanding possible root causes of a myriad of systemic conditions including autoimmune diseases, Lyme disease, chronic fatigue syndrome, heavy metal toxicities; parasitic, candida, mold and other fungal infections.
What Patients Have to Say
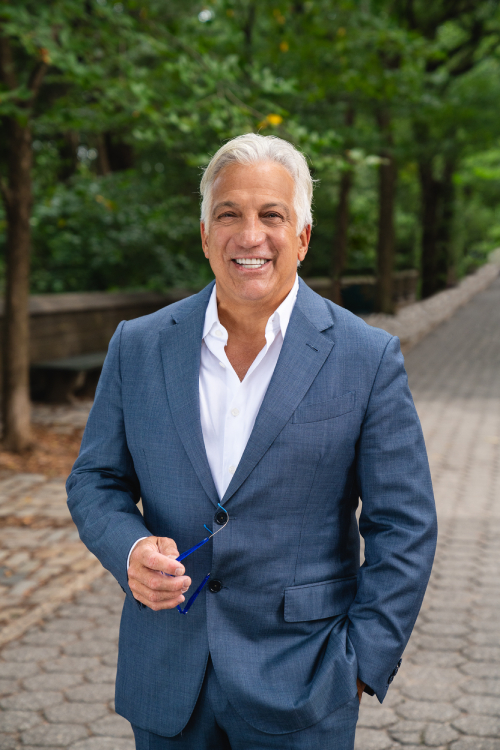
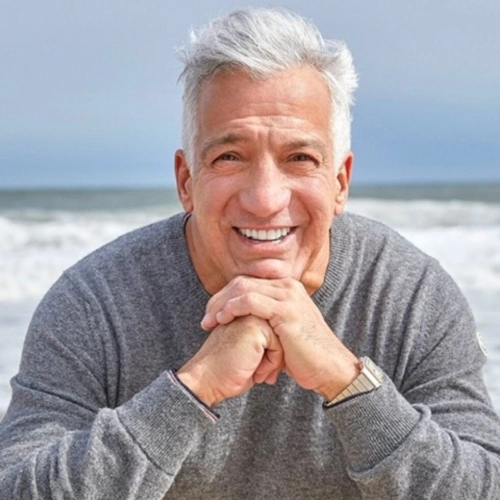
Meet Your Biologic Dental Team