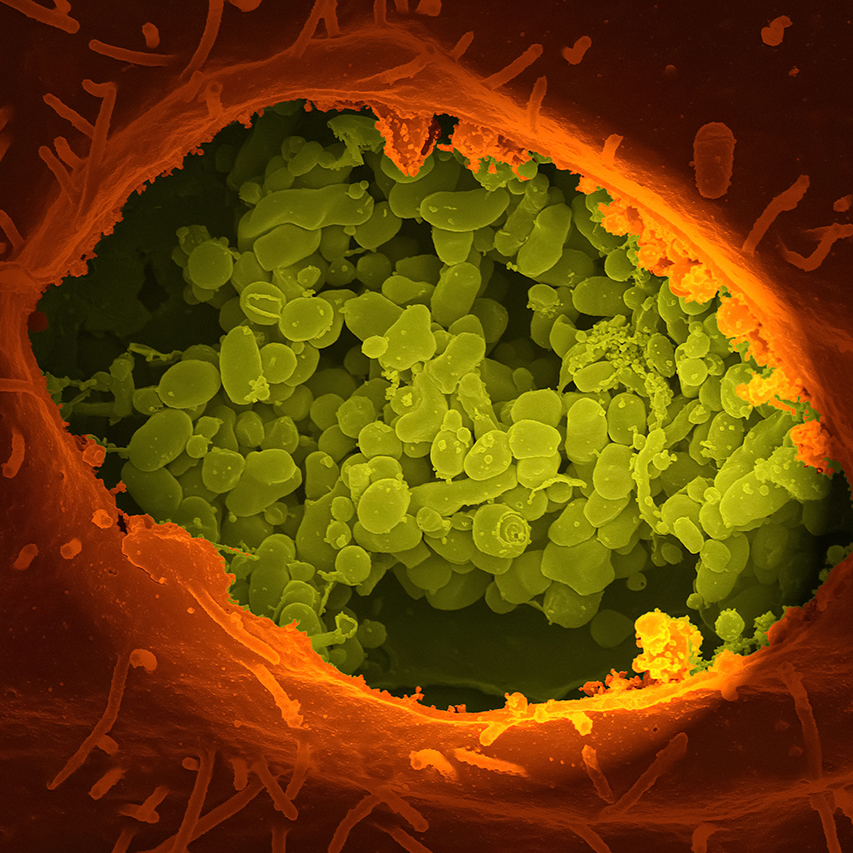
Your body is the host of countless microscopic organisms living in harmony to provide vital functions for your well-being. These complex communities are known as microbiomes, and your mouth is the site of one of the largest microbiomes in your body.
We’ve known for centuries that microbes live in the human mouth. Still, the field of biological dentistry has only recently learned the full extent of what the oral microbiome is and how it impacts your health.
Understanding how to cultivate a thriving oral microbiome is a major key to better health — from your mouth all the way to your toes.
What is the oral microbiome?
The oral microbiome is the collection of bacteria, viruses, and fungi within your mouth. These particles live in your saliva and on every surface of your mouth.
Think of the oral microbiome as a mini-immune system for your mouth. Like the gut microbiome, it houses the organisms that help prevent and heal disease — most often, in the oral cavity.
Second only to your gut, your mouth is the largest and most diverse microbiome in your body. Over 700 species of bacteria and other microorganisms gather in colonies on your teeth, tongue, hard palate, gums — and practically every crevice in your oral cavity.
Genome sequencing using cutting-edge bioinformatics technology has allowed scientists to better understand and characterize microorganisms in the oral microbiome.
These various micro-environments attract and host different bacterial populations made of billions of microbes. Together, they form semipermeable membranes that significantly affect the health of your mouth, gut, and — by extension — the rest of your body.
What’s in a healthy oral microbiome?
Your oral cavity is an intricate habitat of billions of microorganisms, consisting of various types of bacteria, archaea, viruses, fungi, and protozoa. These thrive in the warm, wet environment of your mouth.
Some of the most common bacteria in the oral microbiome include:
- Lactobacilli
- Bifidobacteria
- Porphyromonas gingivalis
- Staphylococci
- Streptococcus mutans (and other Streptococci species)
- Candida
- Veillonella
These bacteria populate a human’s mouth as early as the first days of life.
Some microbial residents come and go when you perform actions like swallowing, coughing, breathing, spitting, and kissing. But in general, these populations remain consistent in healthy individuals.
At any moment, you have billions of microbes living in your mouth.
All bacteria are crucial to your well-being — as long as they’re behaving correctly and their ecosystem is cared for.
However, your oral microbiome can be negatively affected by factors like:
- Smoking tobacco
- Poor diet (high in sugary, processed, and acidic foods)
- Antimicrobial products for the mouth, like most mouthwash
- Poor dental hygiene
What is the purpose of the oral microbiome?
Healthy oral biofilms keep your mouth and body healthy by fighting inflammation and systemic disease.
As part of that overarching purpose, the microbial communities in your oral microbiome:
- Maintain homeostasis within the oral cavity
- Protect the mouth from disease-causing invaders by supplying the appropriate antibodies
- Transport oxygen to the gums
- Remove waste from surfaces of your mouth
- Help to remineralize tooth enamel
- Promote the well-being of all other bodily systems connected to your mouth (which is pretty much every part of your body!)
Functions like these are the benefits of the oral microbiome to prevent oral diseases. But they do much more than that.
The oral microbiome is the gateway from the outside world to your gut microbiome. Each time you swallow, millions of oral microbes are transported from your mouth to your digestive system.
The Oral Microbiome and Dental Health
When the balance of the human oral microbiome is out of balance, we call this a state of dysbiosis. This imbalance can be caused by many factors and show up in familiar ways, such as tooth decay and bleeding gums (gingivitis).
To know if your oral microbiome is healthy, ask yourself if you suffer from oral diseases like cavities, bad breath, and gum disease. If you don’t, your oral microbiome is likely in good shape.
Unlike the gut, the oral microbiome houses many anaerobes responsible for oral infections. The mouth is the primary location for this type of oxygen-independent bacterium, which can also impact overall health.
1. Cavities (Dental Caries)
The relationship between your oral microbiome and dental caries is simple: a healthy oral microbiome should lead to fewer (if any) cavities.
If the homeostasis of your oral microflora is disrupted, Streptococcus mutans can get out of control. This pathogenic bacteria can demineralize even the strongest teeth and cause cavities that require dental fillings.
Unfortunately, caries are one of the most (if not the most) preventable infectious diseases globally, often due to poor oral hygiene and high-carbohydrate diets.
Diseases like dental caries can develop when the biofilm community in your mouth is disrupted by acid-tolerant species.
At Rejuvenation Dentistry, we can use tools like the Sirona cone beam system to accurately assess the condition of your teeth.
2. Gum Disease (Periodontitis)
Inflammation caused by a dysbiotic oral microbiome can affect the soft tissue in your mouth. This allows pathogenic microbes to disrupt the supragingival (above the gum line) and subgingival (below the gum line) communities.
This may even lead to the release of bacteria through the weakened gums into the bloodstream, causing further systemic disruptions throughout the rest of the body.
That’s why it’s important to protect the biofilm in your mouth through proper oral hygiene and nutrition, eliminating dental plaque before it causes problems.
3. Bad Breath (Halitosis)
Holistic dentistry looks at conditions like halitosis to ensure that you’re properly caring for your oral microbiome to avoid the development of bad breath.
Disruption of the microbial community in your mouth causes bad breath — even before you notice the symptoms.
How a Dysbiotic Oral Microbiome May Impact Overall Health
If you’re experiencing problems anywhere within your body — including your mind — chances are that your oral microbiome is imbalanced and disturbing other systems.
That’s because there’s a bi-directional relationship between the health of your mouth and the rest of your body.
As I like to say, the mouth is the gateway and a mirror to the entire body.
Systemic diseases like heart disease, diabetes, and obesity, and more are linked directly to the quality of your oral microbiome. Let’s take a look at the top offenders according to recent microbiome research.
1. Inflammation
Gut and oral microbial communities help keep your health in check. The malfunction of normal oral bacteria operations can lead directly to chronic issues like immune dysregulation.
Chronic inflammation is the cause of many health issues throughout the body. That’s why a dysbiotic human microbiome may lead to serious problems in the cardiovascular, digestive, immune, and nervous systems — including periodontal diseases.
Chronic, low-grade inflammation significantly impairs systemic health over time.
2. Cardiovascular Health
An impaired oral microbiome has a direct, recognized link to the development of cardiovascular disease (CVD). Inflammation also makes CVD worse. Over time, CVD can lead to strokes, high blood pressure, and endocarditis.
If your oral health is poor, atherosclerosis may happen more quickly as fatty deposits build up in the arteries without mouth-gut microbes to properly process the food in your digestive tract.
3. Brain Health
The gut-brain axis links the central and enteric nervous system, which is why your intestinal health has a substantial effect on neurological and cognitive function.
A 2020 study explored the biological correlation between impaired oral microbiota and the development of severe brain disorders such as autism, Alzheimer’s disease, and bipolar disorder.
A scientific study in 2019 identified the bacteria most responsible for gum disease could potentially have a causal (not correlational) link to the development of Alzheimer’s disease.
4. Mental Health
A dysbiotic human oral microbiome can also affect emotional and mental well-being.
As stress harms the microbes in your mouth, the gut-brain axis connection can influence levels of anxiety and depression as early as birth.
5. Diabetes
Sedentary lifestyles and poor diet are primary factors in the development of diabetes. But there is also a strong connection between type 2 diabetes mellitus and poor oral health.
Specifically, developing gum disease appears to drastically increase the risk of developing type 2 diabetes. That’s because gum infections and inflammation are directly triggered when your oral microbiota fail.
6. Obesity
Extensive research suggests that a dysbiotic oral microbiome is one major factor in the development of obesity.
A 2019 study explored the connection between oral microbiome and obesity. Scientists found that multiple oral bacterial taxa were significantly associated with obesity, especially pathogens associated with weight gain during adulthood and above-average BMIs.
Researchers have also observed a connection between oral microbial profiles and obesity in children.
7. Cancer
A 2020 study concluded that certain oral bacterial species are associated with cancer and that poor oral health may play a part in the development of:
- Pancreatic cancer
- Colorectal cancer
- Lung cancer
- Oral cancer
8. Infertility & Pregnancy Complications
Researchers have found significant evidence linking periodontal pathogenic bacteria in the oral microbiome to adverse pregnancy outcomes (APOs) like preterm birth and preeclampsia.
The transmission of pathogenic microorganisms through the mouth can cause a dysbiotic vaginal microbiome state. This may lead to complications like low birth weight, a higher rate of miscarriage, and even infertility.
9. Sexual Dysfunction
The reproductive systems in men and women may be impacted by imbalances in the human microflora.
A 2020 study investigated a potential link between erectile dysfunction and dysbiosis of the gut microbiome. While their findings required further investigation, researchers did notice a remarkable difference in the abundance of Alistipes and Clostridium XVIII bacteria between subjects with and without erectile dysfunction.
Dysbiosis of the human oral microbiome may be connected to Sjögren’s syndrome, characterized by both oral and vaginal dryness.
10. Autoimmune Conditions
Recent research suggests certain features of the oral microbiome are associated with rheumatoid arthritis, an inflammatory autoimmune disease.
HIV/AIDS may also be connected to the state of one’s oral microbiome. As with other autoimmune conditions, there is a noticeable difference in the oral microflora of those with and without HIV/AIDS.
11. Osteoporosis
The development of osteoporosis and periodontitis share many characteristics and risk factors, pointing to a bidirectional relationship between these two conditions.
A 2020 study focused on how oral bacteria triggering inflammation mirrored the progressive loss of bone mineral density. This suggests that one cause and/or risk factor for osteoporosis may be a dysbiotic oral microbiome.
12. Cirrhosis of the Liver
Your liver can be severely damaged if the microbiome in your gut — and, by extension, your mouth — is not well. Chronic liver diseases can lead to permanent scarring.
Scientists have documented a clear correlation between the development of liver cirrhosis and the presence of invasive buccal microorganisms that entered the gut through the mouth.
How to Support Your Oral Microbiome
How can I improve my oral microbiome? To improve your oral microbiome for a thriving mouth-body connection:
- Ditch the antimicrobials in oral hygiene: Stop using astringent, microbe-killing ingredients like detergent-based toothpastes in your oral care routine.
- Eat microbiome-supporting foods: A healthy diet consists primarily of alkalizing, anti-inflammatory, and antioxidant-rich foods. Organic fruits and vegetables, high-quality meats and animal products, and fermented foods and drinks should be the foundation of your dietary habits. These foods promote health, in part, by ensuring your salivary flow is rich with essential nutrients and microorganisms.
- Use oral probiotics: Daily oral probiotics, explicitly designed to increase the commensal (disease-preventing) bacteria in your mouth, can help support a healthy oral microbiome. Some research suggests these targeted supplements can stop disease-causing pathogens that may otherwise cause oral diseases.
- Stay active: Begin a daily regimen of high-intensity exercise, even if you can only set aside 15 minutes on some days. Active movement increases blood circulation, which is integral to boosting your oral health (and overall health in many other ways).
- Reduce your stress levels: Take steps to reduce stress, as it can cause you to grind your teeth and reduce the saliva that keeps your mouth from drying out. Using CBD is a natural way to treat both anxiety and pain.
Grab a copy of my book, The Mouth-Body Connection.
Learn how to take better care of your oral microbiome by reading The Mouth-Body Connection.
For nearly 4 decades, I’ve been uncovering the complexity and magnitude of the symbiotic relationship the human body has with microbes in the oral cavity.
In my book, I provide an easy-to-follow program that will help you restore a healthy oral ecosystem through diet, exercise, proper mouth care, and mental wellness — what I call The Curatola Care Program.
If you live near New York City, I invite you to schedule an appointment to meet with my staff and me at Rejuvenation Dentistry. We have offices in Manhattan and East Hampton, and we’d be happy to help you achieve holistic well-being through proper care of your mouth.